Abstract
Introduction: Racial disparities in survival have been reported for different types of cancer including Hodgkin and non-Hodgkin lymphomas. The underlying mediators of these disparities may include structural racism (defined as census tract disadvantage, affluence, and segregation), treatment patterns, and treatment complications (Abraham IE et al, Blood, 2022). However, there are limited published data regarding racial differences in survival for primary central nervous system lymphoma (PCNSL). The objective of this study was to test the hypothesis that Black patients with PCNSL have inferior relative survival-a measure of disease-specific survival-compared to White patients in the United States.
Method: We conducted a population-based cohort study using the Surveillance, Epidemiology, and End Results-18 database, which includes data from 18 state and local cancer registries in the United States. We included adults aged 18-84 who were diagnosed with PCNSL (including primary intraocular lymphoma) between 2000-2019. We excluded individuals who were diagnosed by autopsy or death certificate. The primary outcome was relative survival, which was estimated by matching individuals with PCNSL to those in the general population by age, sex, year, and race to isolate the excess mortality due PCNSL. Secondary outcomes included overall survival, lymphoma-specific survival, and cumulative incidence of lymphoma-specific death. We tested the study hypothesis using a multivariable flexible parametric relative survival model with Black race as the key independent variable. P values less than 0.05 were considered significant.
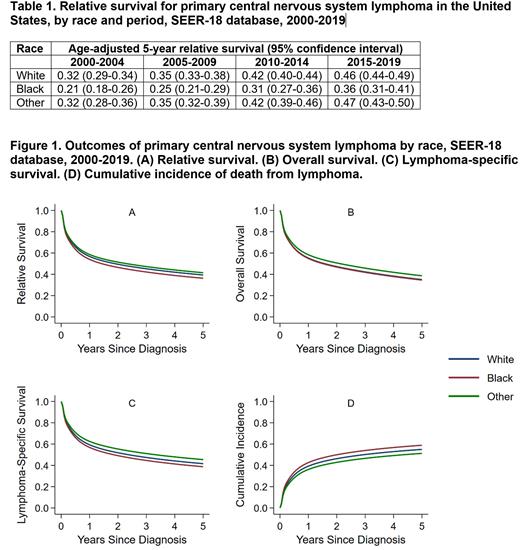
Results: There were a total of 6,545 patients included in the study (White = 5,274, Black = 451, Other = 790, and Unknown = 30). Compared to White patients, Black patients were younger at diagnosis (median age 50 years vs 66 years), had lower median household income (37% vs 27% making <$59,999), were more likely to have a marital status of single (46% vs 16%), and were more likely to reside in the Southern United States (49% vs 19%). Median follow-up was 4.3 years [interquartile range (IQR), 1.6-8.5]. Age-adjusted 5-year relative survival estimates were consistently lower for Black patients across time periods (Table 1). Inferior outcomes were also observed for lymphoma-specific survival and cumulative incidence of lymphoma-specific death (Figure 1). On multivariable analysis after adjustment for age, year, sex, median household income, urbanicity, marital status, geographic region, disease histology, primary site, and B symptoms, Black patients had a 26% higher excess mortality rate compared to White patients (excess hazard ratio, 1.26; 95% confidence interval, 1.09-1.45; P = 0.001).
Conclusion: In this population-based cohort study of PCNSL in the United States, we observed inferior outcomes for Black patients compared to White patients including a 26% higher excess mortality rate after adjustment for potential confounders. Despite the improvement in the 5-year relative survival for Black patients across time periods (2000-2019), it remained lower than White patients. Plausible explanations for these observations include structural racism and differences in treatment patterns and complications. Our study underscores the need for additional research to identify and address the factors leading to racial/ethnic disparities for patients with PCNSL.
Disclosures
Epperla:Incyte: Speakers Bureau; Novartis: Honoraria; TG Therapeutics: Other: Ad Board; BeiGene: Other: Ad Board; Seattle Genetics: Other: Ad Board; Pharmacyclics: Other: Ad Board.
Author notes
*Asterisk with author names denotes non-ASH members.